How To Repair A Hip Fracture With Osteoporosis
Osteoporosis is characterized by a brittle skeleton resulting from decreased os mass.

To maintain strength, cortical bone increases in diameter, just the thickness of the cortex itself decreases.
A larger diameter increases the force of a bone just makes the os vulnerable to rotational and bending forces. Loss of trabecular bone, which arises normally forth lines of stress, likewise decreases the strength of the os. Certain people are susceptible to particular patterns of injury. Of people who sustain a second, contralateral hip fracture, 90% experience the same pattern of injury. This finding indicates that the microtrabecular architecture must exist important.
(top of page)
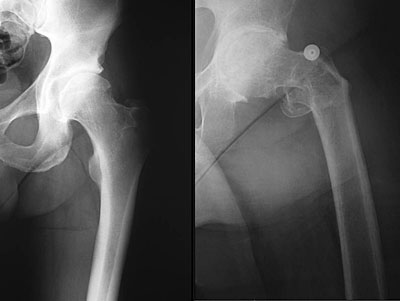
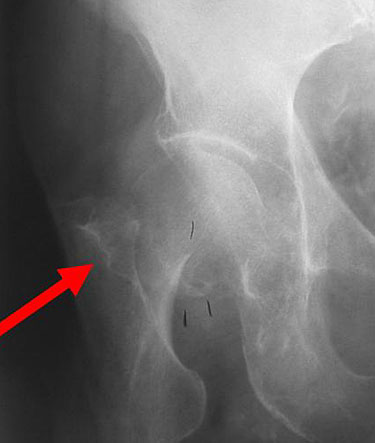
In the elderly, hip pain is usually indicative of a fracture. Pain resulting from a fracture normally presents as onset of groin or upper thigh pain. Depending on the severity of the injury, the patient may or may not be able to walk. Regardless, one must rule out a hip fracture, a pelvis fracture, a spine injury, spinal stenosis, trochanteric bursitis, muscle tears, and knee injuries. The anteroposterior (AP) pelvis view allows the affected and contralateral hips to be compared. The view of the unaffected hip can be used for preoperative planning. A cross-table lateral radiograph should likewise be obtained by flexing the unaffected hip and knee and pointing the x-ray beam at the groin of the affected side. This view places the axle at a correct bending to the femoral neck without manipulation of the afflicted side and reveals any posterior comminution of the femur.

Because plainly radiographs may appear normal or inconclusive, other imaging studies must be considered.Magnetic resonance imaging (MRI) scans are the most sensitive for the evaluation of fractures, particularly occult or nondisplaced fractures. MRI scans can be used immediately afterwards injury and can reveal soft-tissue pathology, such every bit muscle strains, greater trochanteric bursitis, and pelvic fractures.
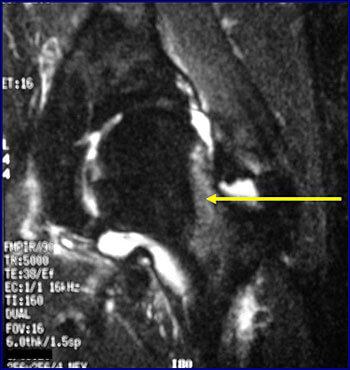
Fracture lines immediately after injury.
Edema in the soft tissues
Radionuclide bone scans that may be used 48 to 72 hours after the injury, are sensitive for metastatic illness. Bones scans are valuable for patients who cannot get an MRI scan.

CT scans reveal fractures only when they are displaced. CT scans are useful for detecting fracture nonunion in the presence of hardware.

(top of page)
There are iii wide categories of hip fractures based on the location of the fracture: femoral neck fractures, intertrochanteric fractures, and subtrochanteric fractures.
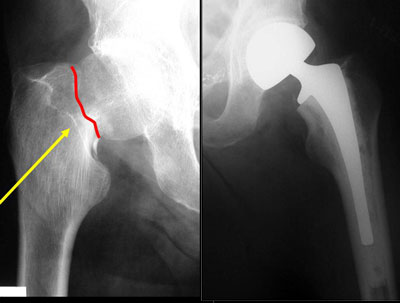
Femoral Neck Fractures
The femoral neck is the most common location for a hip fracture, accounting for 45% to 53% of hip fractures. Per 100,000 person years, approximately 27.7 femoral neck fractures occur in men and 63.3 occur in women. The femoral neck is the region of the femur bounded past the femoral head proximally and the greater and lesser trochanters distally (shown below). A femoral cervix fracture is intracapsular, that is within the hip articulation and beneath the fibrous joint capsule.
Although other, more detailed classification systems be, in general fractures are classified as stable and unstable. Each category has different operative management options.
Treatment of Stable Fractures
Stable fractures are nondisplaced, exhibiting no deformity, or impacted in a valgus positions. Stable fractures may non be detectable on manifestly radiographs, and MRI scanning may be required.
Because nonoperative management results in a secondary deportation rate of 40%, stable femoral neck fractures are generally all-time treated with surgical stabilization and immediate mobilization. Handling is by operative pinning with iii parallel cannulated screws placed adjacent to the femoral neck cortex.

Handling of Unstable Fractures
Unstable femoral neck fractures are displaced and tin be seen on plainly radiographs.
On physical examination, the leg of the afflicted side is externally rotated and shortened; the degree of rotation and shortening varies with the caste of displacement. Displaced fractures in young patients are usually treated with pinning. Pining is chosen considering the risks of arthroplasty, including prosthetic clothing and loosening, are high for immature patients, and their rate of healing is loftier due to the absenteeism of osteoporosis. Equally age and osteoporosis increase, the rate of failure (nonunion, secondary deportation, avascular necrosis) increases.
Hemi- or total joint arthroplasty is associated with a lower rate of echo surgery than internal fixation and is oft the better selection for older patients. Younger patients may opt for screw fixation and hip salvage. In hemiarthroplasty, the acetabular cartilage is left intact and the implant articulates with the acetabulum.
Hemiarthroplasty requires less surgery than a full joint replacement because the acetabulum is not resurfaced. At that place is a smaller risk of dislocation with hemiarthoplasty because it uses a much bigger head size than total hip arthroplasty. In more agile patients, hemiarthroplasty besides has a take a chance of acetabular cartilage clothing and revision to full hip arthroplasty.
Femoral implants tin can exist cemented or cementless, and in that location are many designs of each blazon. Implant fixation can be achieved by the injection of bone cement around the prosthesis or past bony ingrowth into the prosthesis. A bipolar implant has two heads so that motion tin can occur between ane caput and the acetabular cartilage and between the two heads.

In theory, this arrangement helps to reduce acetabular wear and provide increased motility. A unipolar implant has only one large caput that articulates with the acetabular cartilage.
There appears to be no clinical difference between the outcomes of patients with bipolar or unipolar implants in terms of acetabular vesture and hip motion. Compared with unipolar implants, bipolar implants are more than expensive and take an additional interface for prosthetic vesture. Thus, there appears to be no compelling reason to recommend the more expensive bipolar implant over the unipolar for the elderly patient with a hip fracture. If the stem is not well fixed in the proximal femur, either type will fail quickly.
Full joint replacement typically is performed on an agile patient or one with preexisting arthritis. During a total joint replacement, the acetabulum is resurfaced and a metal cup with a polyethylene liner is stock-still inside. Articulation at the hip takes place between the implant's caput and the polyethylene liner.

The determination to treat femoral neck fractures with pinning or with arthroplasty is controversial. The advantages of pinning include less invasive surgery, less blood loss, and less postoperative morbidity. However, treatment by pinning carries a higher run a risk of more surgery in the future. As implied, arthroplasty results in more than acute postoperative morbidity, but information technology offers fewer reoperations for nonunion, hardware failure, and osteonecrosis.
My protocol divides patients into 3 categories: patients with nondisplaced fractures, "low" activity patients with displaced fractures, and "high" action patients with displaced fractures. Nondisplaced fractures are treated with pinning. Displaced fractures in inactive patients are treated with unipolar hemiarthroplasty. Displaced fractures in highly agile patients are treated with total hip replacement.
Treatment Failures
The failures of screw treatment are nonunion and tardily avascular necrosis. Nonunion results primarily from a failure to achieve acceptable mechanical stabilization of the fracture. If the bone does not heal, the screws will slide and backout equally the fracture collapses.

Nonunion typically presents with worsening groin or buttock pain. Tardily avascular necrosis results from insult to the blood vessels that supply the femoral cervix and head. Radiographic monitoring up to three years should detect well-nigh cases of avascular necrosis. The treatment for avascular necrosis or nonunion is hip replacement.
Failure of a hemiarthroplasty results in pain and acetabular erosion. Other complications include dislocation, fracture, and infection. The treatment for a failed hemiarthroplasty is conversion to a total hip replacement.
The failures of a total hip replacement are similar to those of a hemiarthroplasty: loosening, implant vesture, infection, fracture, and dislocation. Handling for a failed total hip replacement is a revision arthroplasty.

(top of section)
(top of folio)
Intertrochanteric Fractures
Intertrochanteric fractures are breaks of the femur betwixt the greater and the lesser trochanters. They are extracapsular fractures that is, outside the hip joint's fibrous capsule.
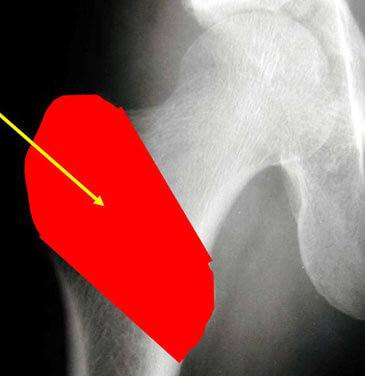
The epidemiology of intertrochanteric fractures is similar to that of femoral neck fractures. Per 100,000 person years, intertrochanteric breaks occur in 34 men and 63 women. Intertrochanteric fractures account for approximately 38% to 50% of all hip fractures.
Many systems of nomenclature, such as the Evans organization, accept been used to describe intertrochanteric hip fractures. However, near systems lack reliability and, in full general, intertrochanteric fractures tin can be divided into two categories: stable and unstable. Stable fractures are those in which the femur is cleaved into ii or three parts. Unstable fractures are those in which the femur is cleaved into four parts or the fracture is of the reverse oblique pattern. Contrary oblique fractures are unstable because of the femur'southward trend to displace medially. This classification method aids in determining what method will be used for fixation.
Two-function fractures have ane fracture line through the intertrochanteric area.
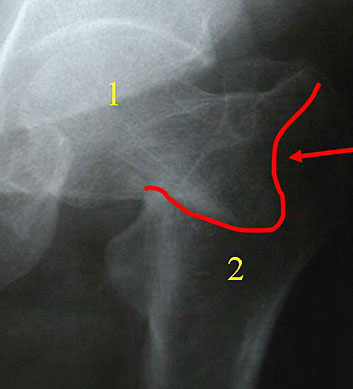
While assessing the stability of a fracture, the most important points to consider are the bone of the lateral buttress and greater trochanter and the bone on the medial side of the proximal femur called the calcar.
Handling of Stable Fractures
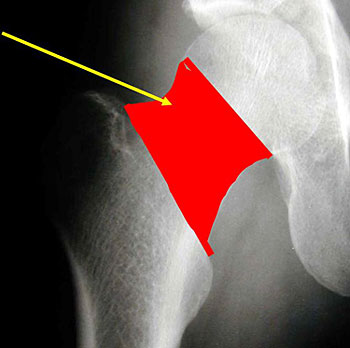
If the fracture is stable, treatment is with a sliding hip spiral coupled to a side plate that is screwed onto the femoral shaft. (shown beneath) The spiral provides proximal fragment fixation. It is set inside a telescoping barrel that allows impaction of the bone, which promotes fracture union. The lateral buttress must be intact so that the spiral will non finish sliding.

A four-function fracture has several fracture lines. The fractured os pieces include: 1) the femoral caput, two) the lesser trochanter, 3) the greater trochanter, and iv) the remaining femur. Fractures with multiple pieces and fracture lines are termed "comminuted". The more pieces, the less stable is the fracture design. Comminution may make fixation with a sliding hip spiral and side plate more than probable to fail.
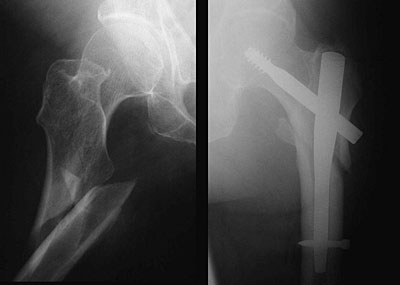
Treatment of Unstable Fractures
Approximately 5% of fractures are extremely unstable, and the direction of the fracture is parallel to the femoral neck. This fracture type is called the reverse oblique pattern. A high rate of failure occurs if the fracture is treated with a sliding hip screw and a side plate. Because of the angle of the fracture, there is no bone laterally to terminate the screw from sliding.
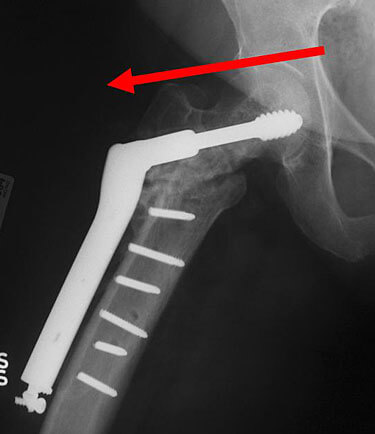
For unstable intertrochanteric fractures, including those of the reverse oblique pattern and those with subtrochanteric extension, an intramedullary hip screw is indicated. This device combines a sliding hip spiral with an intramedullary boom. There are many proprietary varieties, including the Gamma Nail (Stryker, Mahwah, NJ), the Trigen Trochanteric Entry Blast, (TAN nail, Smith and Nephew, Memphis TN) , and the Proximal Femoral Nail (Synthes, W Chester, PA). Intramedullary hip screws can be placed through small incisions, and blood loss may be less than with a hip screw and side plate. The nail acts equally a metal buttress to preclude sliding and provides ameliorate fixation in unstable fracture patterns. No differences take been found between the ii devices in stable fractures.
With a short intramedullary hip screw, the nail does not extend down the full shaft of the femur. Cross-locking of the nail is through a jig, which prevents rotation of the blast within the femur. Short intramedullary hip screws can create a stress riser in the os at the distal spiral.

With a long intramedullary hip spiral, cross locking cannot be done with a jig and must be done freehand under fluoroscopy. Therefore, cross-locking is more difficult. The blast extends throughout the shaft, protecting the rest of the os from futurity fracture.

The hip screw should be placed centrally within the femoral head in the stiff subcortical bone. Evaluation of hip screw placement is made past determining the tip-apex distance under fluoroscopy. The tip-apex altitude is the sum of the distances from the tip of the hip screw to the apex of the femoral head as measured on AP and lateral radiographs

Baumgaertner et al. showed that no fracture had loss of fixation secondary to screw cut-out when the tip-apex altitude was less than 24 mm. When the tip-apex distance was greater than 45 mm, the screw cutting-out charge per unit increased to 60%.
Failure mechanisms of a hip screw include nonunion, screw cutting-out, boom breakage, malunion, and limp. Although sliding of the hip spiral allows for os pinch and hopeful healing, it makes the limb shorten and causes abduction weakness. Most complications are treated with total hip arthroplasty.
Subtrochanteric Fractures
Subtrochanteric fractures are located between the bottom trochanter and the femoral isthmus that is, in the proximal office of the femoral shaft.
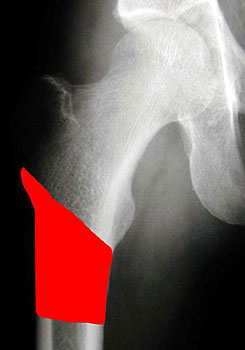
They are less common than femoral neck and intertrochanteric fractures, accounting for approximately 5% to xv % of hip fractures. Subtrochanteric fractures are less stable than the other two types of hip fractures and, consequently, more difficult to fix.
Treatment
A subtrochanteric fracture is treated with an intramedullary hip screw.
No lateral buttress exists in a subtrochanteric fracture and, therefore, sliding hip screws with side plates provide poor fixation. After surgery for a hip fracture, weightbearing should be allowed equally tolerated. It has been shown that patients with less stable fracture patterns protect themselves by self-restricting weightbearing and move.
(top of section)
(height of folio)
In summary, the type of fracture determines the blazon of surgery. Patients with femoral neck fractures are treated with pinning or hip arthoplasty, depending on the age of the patient and the presence and degree of displacement. Patients with intertrochanteric fractures are treated with a sliding hip screw or an intramedullary hip screw, depending on the stability and location of the fracture.
(summit of folio)
•Apple DF Jr, Hayes WC, editors. Prevention of Falls and Hip Fractures in the Elderly. Rosemont (IL): American Academy of Orthopedic Surgeons; 1993.
•Baumgaertner MR, Curtin SL, Lindskog DM, and Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Articulation Surg 1995;77A(7):1058-1064.
•Cummings SR, Rubin SM, Blackness D. The hereafter of hip fractures in the United States. Numbers, costs, and potential furnishings of postmenopausal estrogen. Clin Orthop Relat Res 1990;252:163-166.
•Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: a greater risk of morbidity and bloodshed in men. J Orthop Trauma 2005 Jan;nineteen(1):29-35.
•Koval KJ, Sala DA, Kummer FJ, Zuckerman JD. Postoperative weight-bearing later a fracture of the femoral neck or an intertrochanteric fracture. J Bone Joint Surg 1998; 80A(3):352-356.
•Koval KJ, Zuckerman JD. Hip fractures. I: Overview and evaluation and treatment of femoral-cervix fractures. J Am Acad Orthop Surg 1994;ii(3):141-149.
•Lofman O, Berglund Chiliad, Larsson 50, Toss G. Changes in hip fracture epidemiology: redistribution between ages, genders and fracture types. Osteoporos Int 2002;xiii(1):18-25.
•Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality hazard after hip fracture. J Orthop Trauma 2003;17(i):53-56.
•Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the 2nd hip fracture. Clin Orthop Relat Res 1993;289:166-169.
(top of page)
Source: https://www.hopkinsmedicine.org/gec/series/fixing_hip_fractures
Posted by: byrdbefer1969.blogspot.com


0 Response to "How To Repair A Hip Fracture With Osteoporosis"
Post a Comment